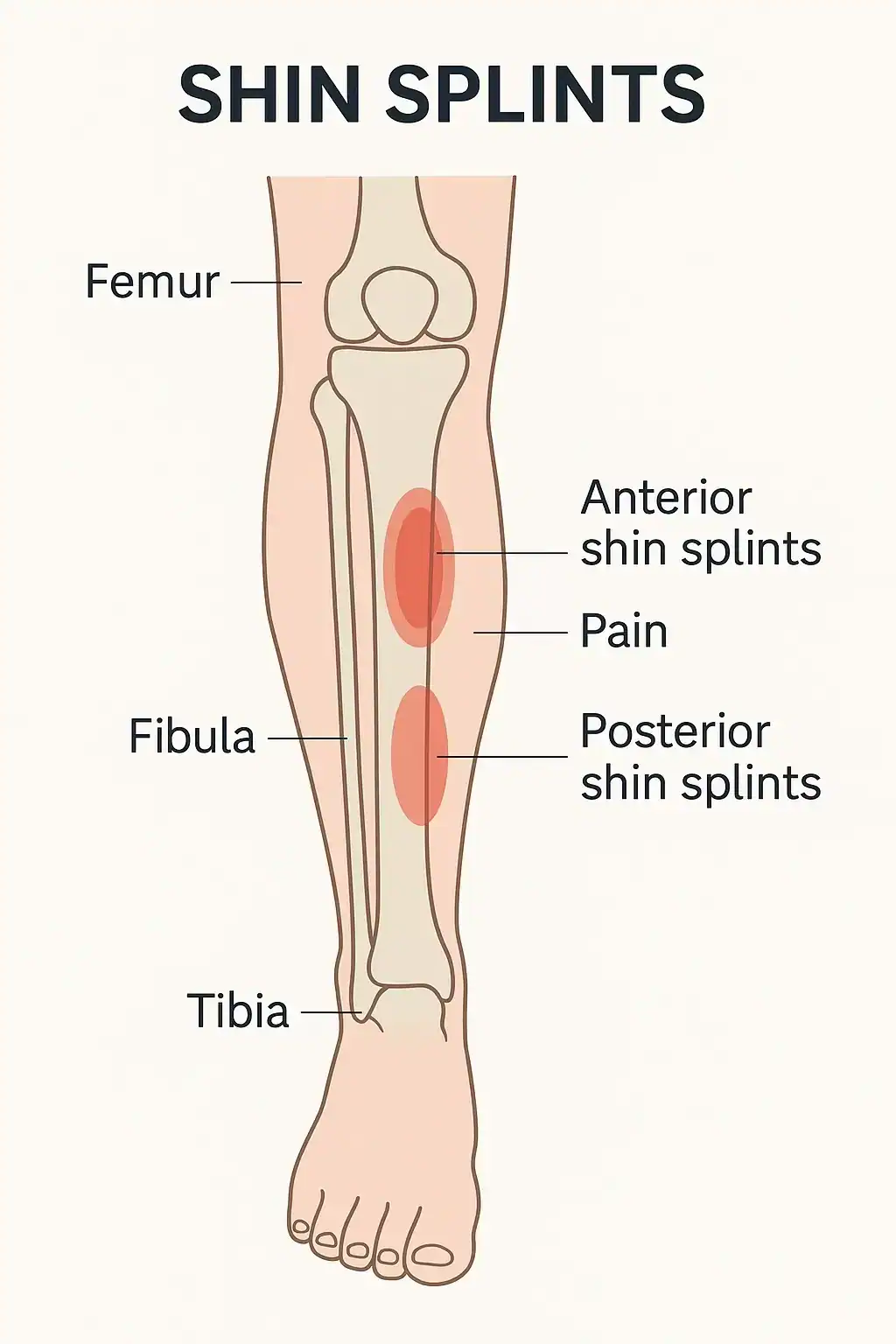
Shin splints are a common overuse injury that causes pain along the shinbone (tibia), usually on the inner edge of the lower leg. They often affect runners, dancers, and people who suddenly ramp up physical activity. The discomfort comes from stress on the muscles, tendons, and bone tissue around the shin. You can find a medical overview from the American Academy of Orthopaedic Surgeons here and additional clinical insight from the Mayo Clinic.
Are Shin Splints the Same as Medial Tibial Stress Syndrome?
Yes—when most people say “shin splints,” they are usually referring to medial tibial stress syndrome (MTSS). MTSS is the medical term for pain and inflammation along the inner edge of the tibia (shinbone) caused by repetitive stress. It’s the most common form of shin splints, particularly in runners, dancers, and military recruits.
However, “shin splints” is sometimes used as a general term for any exercise-related shin pain. That means not all shin pain qualifies as MTSS. Other potential causes include stress fractures or exertional compartment syndrome, which require different treatment.
If you’re unsure whether your pain is from MTSS or something more serious, it’s best to get a diagnosis from a healthcare provider.
Causes of Shin Splints
Several contributing factors can lead to the development of shin splints. The condition often results from repetitive activity and biomechanical stress.
- Rapid increase in exercise intensity or frequency
- Running or training on hard, sloped, or uneven surfaces
- Wearing unsupportive or worn-out shoes
- Flat feet or abnormal gait mechanics
- Weak hip, core, or lower leg muscles
Symptoms
People with shin splints typically feel a dull, throbbing, or aching pain along the front or inside of the shin during or after exercise. The pain may start gradually and intensify if activity continues. Other possible symptoms include:
- Tenderness along the shinbone
- Slight swelling in the lower leg
- Discomfort that worsens with impact activities like running
Diagnosis for Shin Splints
Doctors typically diagnose shin splints through a combination of physical examination, medical history, and a discussion of your recent physical activity. During the exam, the physician may press along the shinbone to check for areas of tenderness, swelling, or pain. They’ll also assess your range of motion, gait, and foot structure to identify any contributing biomechanical issues.
A key part of the diagnosis involves ruling out more serious conditions that mimic shin splints, such as stress fractures or chronic exertional compartment syndrome. If symptoms are severe, persistent, or focal—meaning the pain is concentrated in a specific area—your doctor may order imaging tests:
- X-rays help detect bone abnormalities or small fractures that may not be felt during a physical exam.
- MRI (Magnetic Resonance Imaging) can reveal stress fractures, soft tissue damage, and inflammation in the surrounding muscles and periosteum.
- Bone scans are occasionally used to differentiate between shin splints and a stress fracture when other tests are inconclusive.
These tests aren’t always necessary but can be essential when rest and conservative care fail to improve symptoms. An accurate diagnosis ensures the right treatment plan and helps prevent complications or recurrence.
Treatment Options
Treating shin splints focuses on rest and reducing strain on the lower legs. Most cases resolve with conservative care. Helpful treatment approaches include:
- Rest and activity modification
- Applying ice packs for 15–20 minutes at a time
- Using anti-inflammatory medications if recommended
- Gentle stretching of calves and Achilles tendon
- Physical therapy for gait correction or strengthening
When to See a Doctor
If the pain is sharp, localized, or doesn’t improve with rest, it could be a sign of a more serious condition like a stress fracture. Seek medical advice if symptoms persist for more than a couple of weeks or if swelling or numbness occurs.
Prevention Tips
There are simple strategies to help reduce your risk of shin splints and support your legs during high-impact exercise.
- Build up mileage or training time slowly
- Wear cushioned, supportive footwear with proper arch support
- Stretch calves, ankles, and hamstrings before and after workouts
- Cross-train with low-impact exercises like cycling or swimming
- Replace running shoes every 300–500 miles
For more information on protective footwear, check out this guide to the best running shoes for shin splints.
Common Questions About Shin Splints
Here are common questions about shin splints (or medial tibial stress syndrome) and their answers.
Shin splints cause diffuse pain across a broader area of the shin, while stress fractures usually cause sharp, localized pain in a specific spot.
It’s generally not recommended. Continuing high-impact activity can make the condition worse or lead to a more serious injury.
No. Dancers, military recruits, and people who do high-impact interval training can also develop shin splints.
With proper care, shin splints typically heal within 2 to 6 weeks. Rest and rehab are key to recovery.
Supportive shoes with adequate cushioning and stability can reduce the impact on your legs. Look for pairs tailored to your gait and arch type. See best shoes for shin splints.