Last Updated on May 23, 2025 by Andy Walker
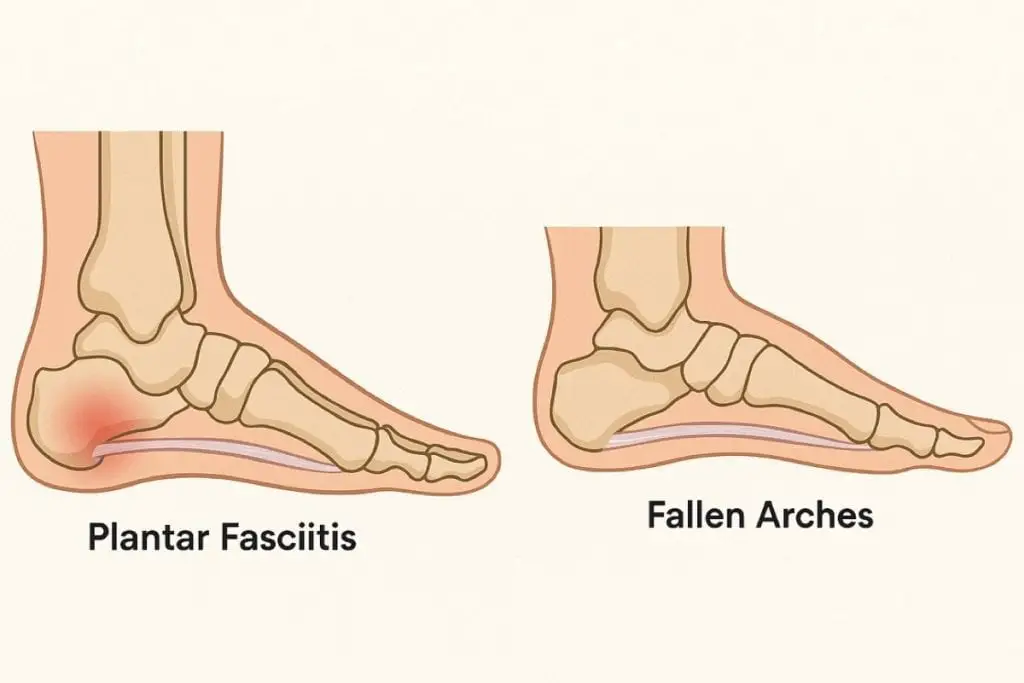
If you’re struggling with pain along the inside of your ankle or noticing your arch is collapsing, you might be dealing with posterior tibial tendon dysfunction (PTTD). It’s one of the most common causes of adult-acquired flatfoot (and so it is also common among avid runners and walkers), but it’s often confused with plantar fasciitis, a different condition that affects the bottom of your foot. Understanding the difference between fallen arches and plantar fasciitis is key to getting the right diagnosis—and the right treatment—before the problem gets worse.
While both cause arch pain for active people, they are very different in terms of cause, symptoms, and treatment. This article will help you understand the difference, so you can choose the right recovery plan and get back on your feet without unnecessary frustration. Ready? Let’s explore these foot issues.
What Is Posterior Tibial Tendon Dysfunction (PTTD)?
PTTD is a condition where the posterior tibial tendon—which connects the calf muscle to the inside of your foot—becomes inflamed, stretched, or torn. This tendon plays a major role in maintaining your foot’s arch. When it weakens or fails, the arch collapses and flatfoot develops, often accompanied by pain and instability.
Symptoms for PTTD include:
- Pain and swelling along the inside of the ankle
- A flattening of the arch that worsens over time
- Difficulty standing on your toes or doing heel raises
- Discomfort during walking or prolonged standing
- Rolling of the ankle inward (overpronation)
PTTD often develops gradually and is most common in adults over 40, though it can affect younger people who overtrain or wear unsupportive shoes.
See also: Cleveland Clinic page on this topic
What Are Fallen Arches?
Fallen arches—also known as flat feet—occur when the arch of the foot flattens, either partially or fully. Some people are born with flat feet, but in many cases, it develops over time due to aging, weight gain, injury, or weakening of the posterior tibial tendon.
PTTD is one of the most common causes of acquired flatfoot. For a deeper dive into symptoms, causes, and treatment approaches, explore our full guide to flat feet.
What Is Plantar Fasciitis?
Plantar fasciitis is a separate condition that involves inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot from heel to toe. It’s one of the leading causes of heel pain and is especially common among runners, people with tight calves, or those who spend hours on hard floors.
The pain of plantar fasciitis is usually sharp, centered in the heel or arch, and worst with your first steps in the morning. It tends to improve with movement throughout the day. For a full overview of symptoms and recovery, read our plantar fasciitis guide.
See also this video:
How PTTD and Plantar Fasciitis Differ
Although these conditions can both cause arch pain, they affect different tissues and have different symptoms.
Pain location is one of the biggest clues. Plantar fasciitis pain is typically under the heel or along the bottom of the arch. PTTD, in contrast, tends to cause pain and swelling along the inside of the ankle and may extend into the arch.
The pain sensations also differ. Plantar fasciitis often causes sharp or stabbing pain when standing up after rest, while PTTD pain is more of a dull ache or burning sensation that worsens with activity. If your foot appears flatter than it used to or rolls inward as you walk, that’s another sign that PTTD may be the issue.
Another important distinction is how quickly the pain responds to rest. Plantar fasciitis often improves quickly with unloading. PTTD pain is slower to resolve and may persist unless the arch is properly supported.
How to Know If You Have PTTD
You don’t need imaging to suspect PTTD. Many physical therapists use simple in-clinic tests to confirm the condition.
The single heel raise test is one of the most reliable: try standing on one foot and lifting your heel. If you can’t do this without pain or your arch flattens as you try, PTTD is likely.
Look at your arch while standing. Has it dropped noticeably? Is one foot flatter than the other? Is your heel rolling inward? These visual signs, combined with inside-ankle pain during or after walking, strongly suggest posterior tibial tendon dysfunction.
How to Treat PTTD at Home
PTTD doesn’t go away on its own, but it’s very treatable when caught early. A focused, consistent home program can help you avoid surgery and restore function.
The most important first step is to reduce strain on the posterior tibial tendon. A support brace that mimics physical therapy taping can immediately reduce pain while helping to prevent further collapse. The Loft 2 Brace is one example that’s been developed specifically for conditions like PTTD.
Daily foot massage, particularly in the arch and around the ankle, can reduce tension and stimulate healing. Use a firm massage tool or ball to work the area for several minutes each day.
A guided strengthening program targeting the calf, ankle, and foot muscles is essential for long-term recovery. This helps rebuild the support structure around the tendon and prevents recurrence.
Gradually return to activity. Don’t jump back into long walks or intense exercise. Instead, increase walking time and standing tolerance slowly, tracking pain and performance.
Shoes are also a major part of PTTD recovery. Choose footwear that offers strong arch support, structured heel counters, and stability features. For performance options, explore our expert picks for the best running shoes for flat feet, which are designed with overpronators and arch support in mind.
If PTTD Isn’t Treated
If PTTD goes unchecked, it can become a progressive condition. Over time, the arch collapses further, leading to rigid flatfoot, arthritis, and ankle joint damage. Pain becomes chronic and can spread up the kinetic chain, affecting knees, hips, and back.
That’s why it’s so important to address symptoms early—even if they seem minor. With consistent support, exercise, and recovery strategies, most cases can be reversed or stabilized without invasive treatments.
Take Charge of Your Arch Pain
Posterior tibial tendon dysfunction is a treatable but serious condition. It requires a different approach than plantar fasciitis or general flat feet. If you’re dealing with pain on the inside of your ankle, progressive flattening of the arch, or difficulty standing on tiptoe, don’t assume it’s just overuse or a bad shoe day.
With the right treatment approach—targeted support, strengthening, massage, and smart footwear—you can rebuild your arch support and reduce your symptoms dramatically.
Start by taking the right steps. Use a brace to offload the tendon. Follow a structured strengthening program. And wear shoes that help—not hurt—your recovery.
Need help figuring out what shoes to wear or how to start recovery? Use our site’s free resources, or explore our expert-tested guides on flat feet and plantar fasciitis to get personalized tips and recommendations.